There is currently no accurate way to predict an individual’s course of multiple sclerosis (MS) as the condition varies greatly between individuals. Some people may feel and seem healthy for many years after a diagnosis, while others may progress more quickly.
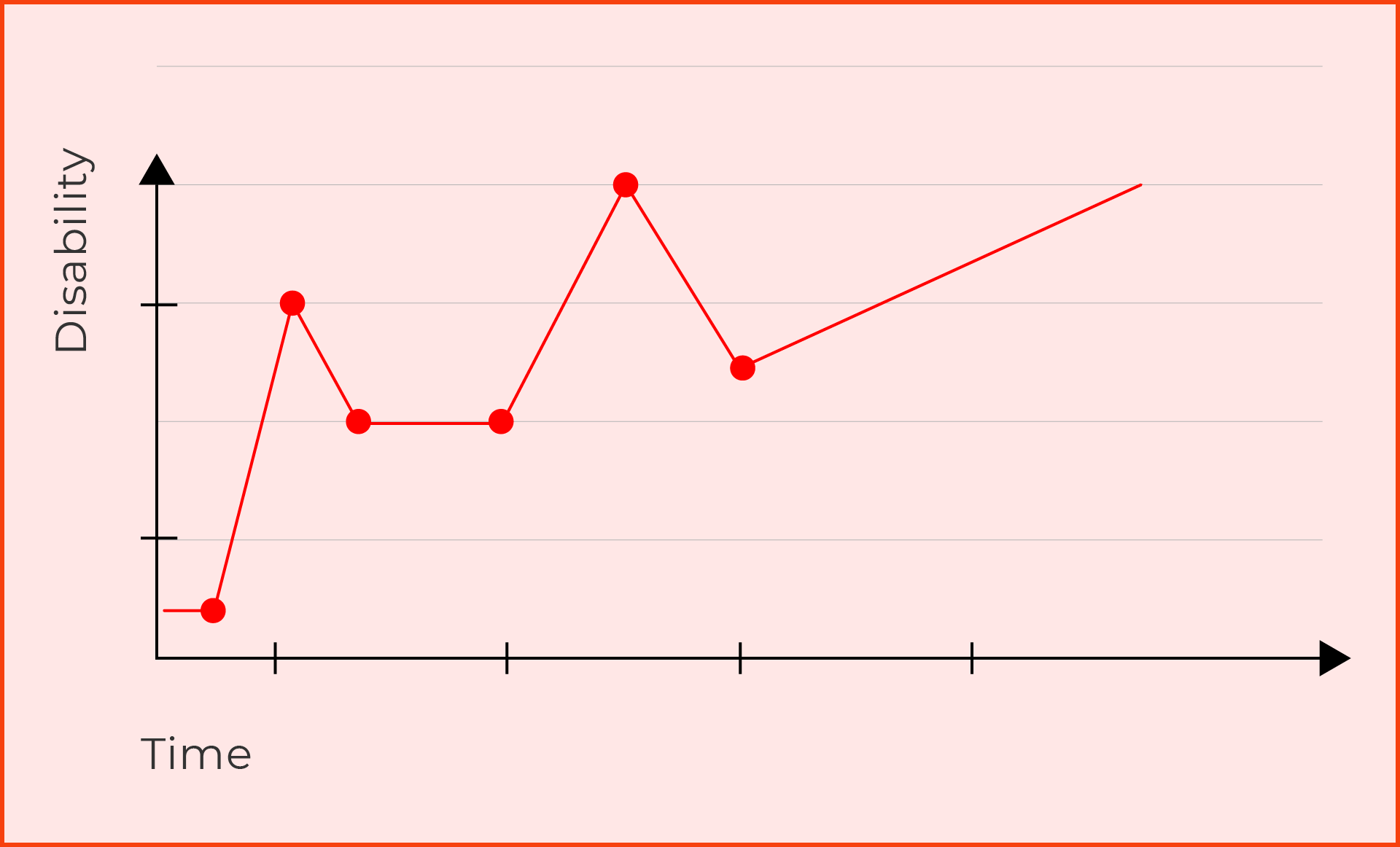
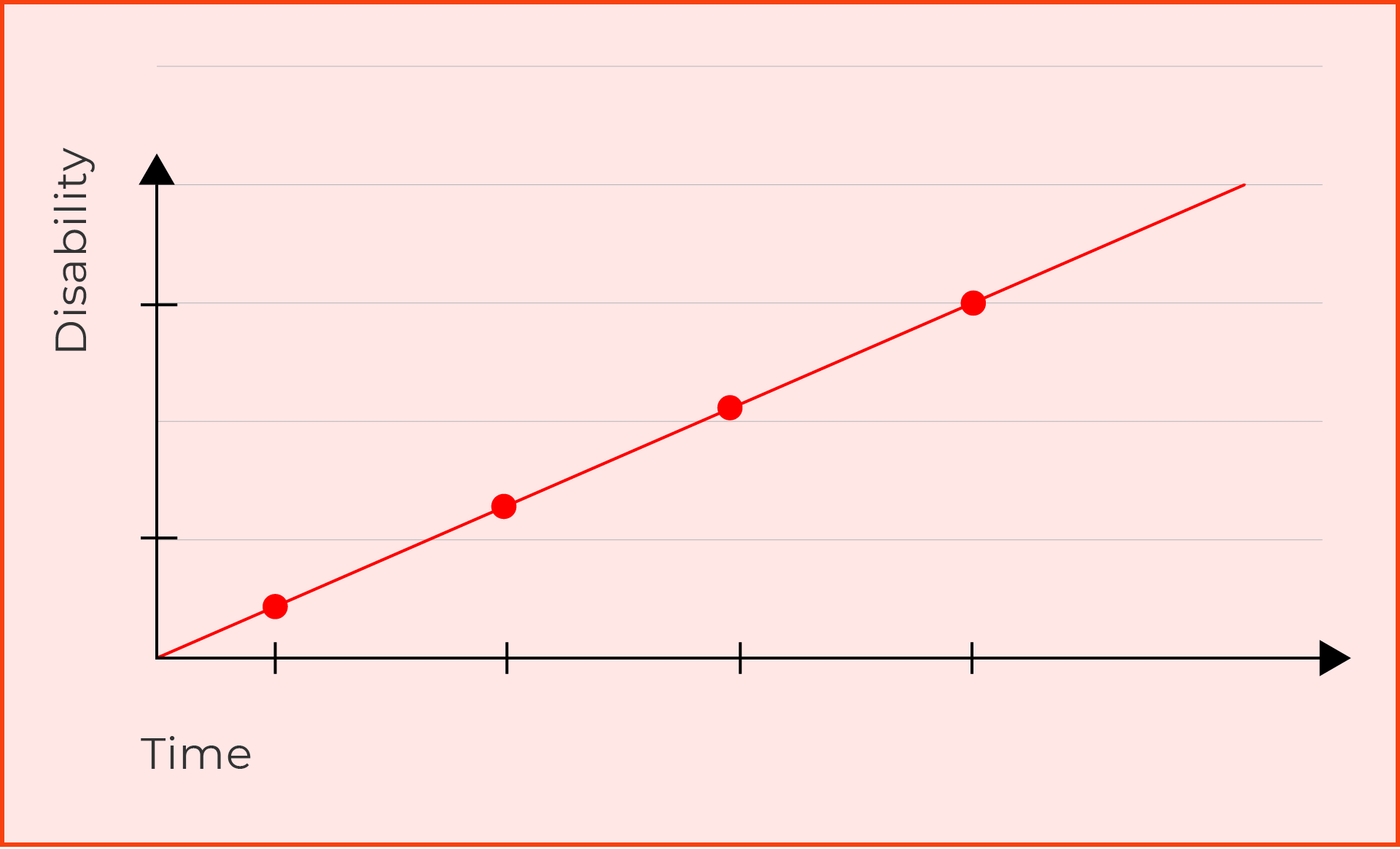
There are three main types of MS: relapsing remitting MS (RRMS), secondary progressive MS (SPMS) and primary progressive MS (PPMS). The classification of disease depends on its activity and progression.
Identifying the type of MS is important in order to consider the most appropriate disease modifying therapy (drug treatment) for each individual and to assist in the many clinical decisions that need to be made following diagnosis. In recent years, there has also been a focus on whether the MS is active (unstable, a relapse or new MS lesions on MRI) or inactive (stable, no relapses, no new lesions on MRI) to guide treatment and management decisions.
Relapsing Remitting MS is the most common form of MS. About 85% of people with MS are diagnosed with RRMS. It is caused by flare ups or exacerbations of the neurological symptoms of MS, also known as relapses, followed by periods of recovery or remission.
For some people, before a diagnosis of RRMS is made, they may be first diagnosed with clinically isolated syndrome (CIS). This is essentially the first presentation of MS (the first relapse), but a diagnosis cannot be confirmed until a second episode occurs, or new lesions develop in the central nervous system to fulfill the “multiple” component of MS. It is caused by inflammation and demyelination in the central nervous system, but not everyone who experiences CIS will develop MS. It is unknown why CIS develops into MS for some people and not for others.
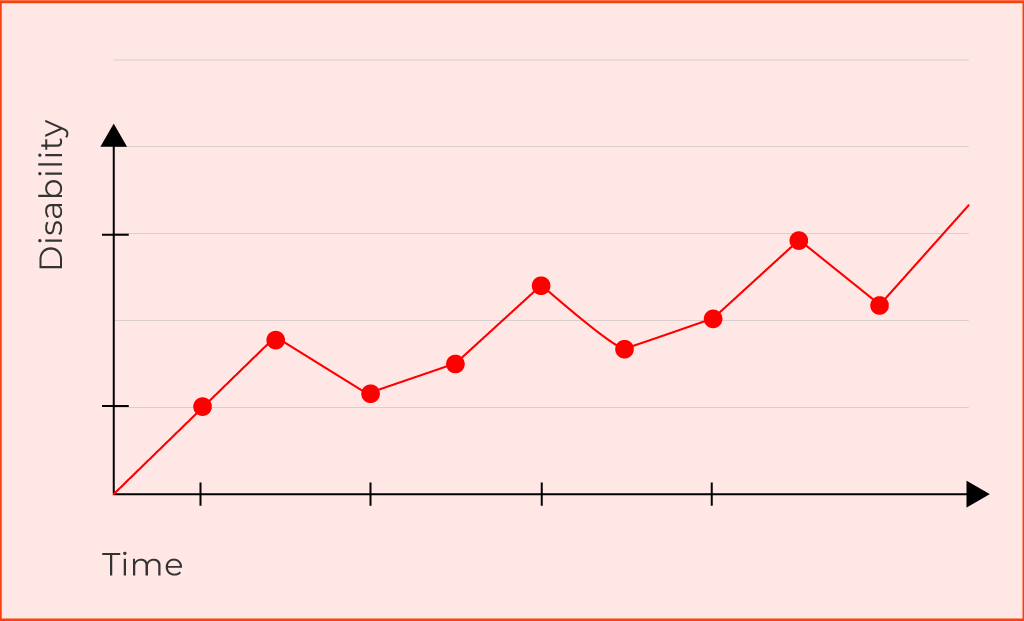
Secondary Progressive MS is a secondary phase of relapsing remitting MS that can develop years to decades following the initial onset of symptoms. SPMS is characterised by a reduction in relapses and a progressive worsening of symptoms (accumulation of disability) over time, with no obvious signs of remission.
Primary Progressive MS is diagnosed in approximately 10-15% of people with MS. PPMS is characterised by a progressive worsening of symptoms and disability right from the beginning, without periods of recovery or remission. Relapses for most people are possible, but not common. Additionally, there can be periods of “plateau” where progression can stabilise for a period of time.
The road to diagnosis can be remarkably fast for some people and discouragingly slow for others. Central to diagnosis is a thorough medical history detailing all symptoms, a clinical neurological examination and a good quality magnetic resonance imaging scan (MRI) of the brain and spinal cord.
There are specific international guidelines used by the neurologist that govern the diagnosis of MS, to enable an accurate and faster diagnosis. This is known as the McDonald criteria. Additionally, blood tests are used to rule out other similar diseases which can mimic MS.
Other tests can be used in conjunction with MRI to confirm the diagnosis, such as electrophysiological tests of the limbs and eyes (nerve conduction tests), specific eye tests (optical coherence tomography/OCT) or a lumbar puncture (spinal tap) to look for specific cells in the cerebrospinal fluid.
For a comprehensive overview of how MS is diagnosed, click here.
A relapse is a sudden onset of new neurological symptoms, or significant worsening of existing MS symptoms. Relapses are also known as “episodes”, “exacerbations” or “flare-ups”. No two relapses are alike, and symptoms vary from person to person and from one relapse to another.
Some relapses produce only one symptom (related to inflammation in a single area of the central nervous system) while other relapses cause two or more symptoms at the same time (related to inflammation in more than one area of the central nervous system). They can range from mild to serious in severity.
To be medically considered a relapse, it must last at least 24 hours and be separated from the previous relapse by at least 30 days. There should be no other possible cause for the relapse, such as infection, recent surgery or overheating. Most relapses last from a few days to several weeks or even months.
Managing a relapse varies from person to person and will depend on the severity and location of the attack. If you think you are experiencing a relapse, talk to your neurologist, MS Nurse or GP as soon as possible. Relapses can be a sign that your MS is active so it’s important to report each one, even if you don’t think you need medical treatment.
For a comprehensive overview of managing a relapse, visit our symptom page.
Managing MS depends on your individual circumstances, and the type of MS you have been diagnosed with. MS can change over time as well, so it’s important to talk with your neurologist, MS Nurse or GP as soon as you notice any changes. Your healthcare team will also work with you to create an individualised MS management plan.
In general, managing MS involves a mix of symptom management and disease modifying therapies.