A number of important biological processes contribute to disease in MS, including inflammation and neurodegeneration (nerve loss). While inflammation is reasonably well understood and treatable with current drugs, neurodegeneration is more complex, poorly understood and only responds to treatments in a very limited manner. Neurodegeneration is also thought to underlie progression of MS. The burning question, therefore, is: what is the cause of nerve loss?
Recent scientific evidence shows that blood particles known as ‘platelets’ play an important role in autoimmune diseases such as MS. Platelets are small cell fragments that are important in blood clotting, but also have wider functions, including the capacity to exacerbate inflammation in laboratory models of MS.
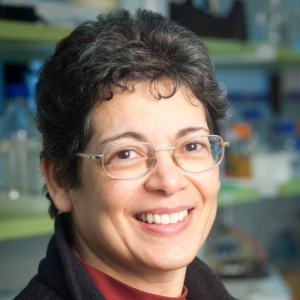
Dr Orian’s research has shown that the role of platelets goes even further and that these particles are key drivers of the autoimmune process and might be responsible for both inflammation and neurodegeneration. She suspects that platelets, rather than immune cells, cause nerve loss and that targeting platelets in early disease may slow down some of the degeneration of nerves in MS, thereby potentially delaying progressive MS.
The overarching aim of this project is to demonstrate that platelet-targeting is both anti-inflammatory and neuroprotective in MS, using a novel platelet-targeting drug. This will provide proof-of-concept for the potential of platelet-targeting therapies to treat MS.
Dr. Jacqueline Orian and her team have made significant progress in their research in MS. They developed a new laboratory model that better represents the disease and confirmed the entry of platelets into the brain and spinal cord. By studying this model, they found that platelets are associated with brain cells and contribute to inflammation and nerve cell death.
Using a novel drug that targets disease-associated platelets, they demonstrated in laboratory models of MS that this drug halted disease progression, promoted remyelination, and provided neuroprotection. These findings show promise for platelet-targeting therapies in treating MS and improving mobility.
The early targeting of platelets with the drug has shown positive outcomes, even in the most severe of models. The drug also restores platelets to a normal state in the circulation, ensuring its safety.
The findings from this research have been presented at national conference and submitted for publication in peer reviewed scientific journals, one of which is in press.
Dr. Orian's research offers hope for platelet-targeting therapies as a breakthrough in MS treatment. These therapies have the potential to prevent disease progression, promote neuroprotection, and restore myelin, leading to improved outcomes for people living with MS.
Updated: 31 March 2023
Updated: 19 January, 2021
Laboratory research that investigates scientific theories behind the possible causes, disease progression, ways to diagnose and better treat MS.

Research that builds on fundamental scientific research to develop new therapies, medical procedures or diagnostics and advances it closer to the clinic.

Clinical research is the culmination of fundamental and translational research turning those research discoveries into treatments and interventions for people with MS.

