In the past decade a number of treatments for MS have become available. Many of these target cells in the immune system. However, determining which treatment would be best for each individual with MS can require some trial and error before the disease is most effectively controlled.
In a recent international study involving investigators from the MS Research Australia-supported Australian New Zealand MS Genetics Consortium (ANZgene), the activity of a known MS risk gene, ZMIZ1, in people with and without MS was investigated. The researchers found that the gene may provide a potential marker for disease activity which could ultimately be used to help guide treatment decisions.
Although this gene had been identified as a potential player in MS, the exact role of the gene and how it might contribute to MS is unclear. It is known to be a type of gene that acts as a master regulator, controlling the function of other genes, which in turn, regulate the function of immune cells.
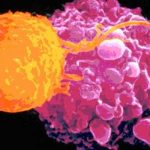
To investigate this, the research team took blood and DNA samples from people with and without MS to see how the gene was behaving differently in MS and how it affected the function of immune cells. The team found that there is less of the gene in the blood of people with MS compared to people without MS. When they subdivided the blood into the different types of immune cell types they found that gene in question was specifically lower in one particular type of immune cell in people with MS.
They also found that the activity of over 1500 genes was, in turn, linked to the activity of the risk gene, with 27 of these genes being common in the samples from all the sites studied. These 27 genes are expressed at different levels in several different types of inflammatory immune cells in people with MS compared to people without MS.
The researchers also looked at how the ZMIZ1 gene interacts with some of the environmental factors known to play a role in MS. For example, low levels of vitamin D and the Epstein Barr Virus (that causes glandular fever) have been linked to the risk of developing MS. The researchers found that some types of immune cells increased their production of the gene in the presence of vitamin D and EBV. This finding indicates that the gene may be a key regulator that integrates different types of information to affect immune system function.
Importantly, the research team also found that ZMIZ1 levels in people with MS were restored to the same levels as people without MS following treatment with fingolimod and dimethyl fumarate. This suggests ZMIZ1 could provide a marker to rapidly show whether treatments are working.
Building up this picture of how this MS risk gene functions in the immune system and how it may respond to the environmental factors and medications that influence MS, helps us to understand how we might ultimately target the right immune cells to prevent MS relapses without broadly suppressing the immune system.